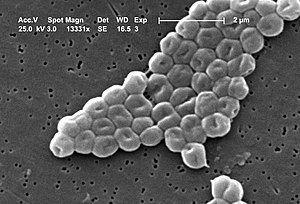
(Methicillin-resistant Stapholococcus aureus, otherwise known as MRSA)
The question of whether humans are increasing bacterial "evolvability" is addressed by two Australian researchers in a review article published in the latest issue of Trends in Ecology and Evolution. They define "evolvability" as "an increased potential for evolution," which can be driven by characteristics such as basal mutation rate, recombination rates, protection against the incorporation of foreign DNA into the genome, and propensity for lateral gene transfer (or acquiring genes from a source other than a "parent"). All of these traits "affect the rate at which genetic variation can be generated"--and some of this variation could very well confer resistance.
Interestingly, many antibiotics were originally isolated from soil bacteria, which probably developed these compounds for use in signalling or competition with neighbors. For cells to survive in these potentially toxic environments, they had to evolve resistance genes alongside those producing poison, and so the terrestrial environment is probably already teeming with genetic elements offering protection from various man-made drugs. Once our antibiotic runoff reaches these environments, bacteria without the genes die off, while those with them will survive, passing on the resistance not only to their "offspring" but also, potentially, to their neighbors. Cells with higher levels of evolvability will become resistant more quickly; in other words, exposure to antibiotics leads not only to the selection of resistance, but also of the ability to develop it. This process works so well that the number of antibiotic-resistant genetic elements has increased significantly over the years. Many such elements are located in wild animals or environments not directly exposed to antibiotics, strongly suggesting that resistance has spread along a bacterial supply chain that begins in anthropogenic environments and extends even into those otherwise considered "pristine."
The authors point out that evolvability is not always a useful characteristic for bacteria to possess. For instance, while some mutations can be advantageous, others can impair functionality or even remove it altogether; likewise, incorporation of DNA from an unrelated bacterium might result in the transcription of a useful protein, but it also could generate something that is ultimately toxic. Thus, we should expect evolvability to be high only in systems where it's a gamble that, more often than not, pays off. This describes the current state of affairs in both terrestrial and aquatic ecosystems, into which humans dump vast quantities of antibiotics each year--especially in the form of waste water. The exact amounts are difficult to measure, but are likely to be large if they are even a small portion of the millions of metric tons produced annually.
(Acinetobacter baumannii, a gram-negative bacterium that is sometimes known as "Iraqibacter" because of its prevalence among US soldiers wounded to Iraq.)
One particularly frightening aspect of the spread of resistance is how it can often involve whole suites of genes rather than just one. Acinetobacter baumannii, for instance, now possesses a "resistance island" containing 45 genes for antibiotic/antimicrobial resistance, as well as resistance to heavy metals such as mercury and arsenic. As a result, A. baumannii infections have become a much greater threat to human health over the last several decades; additionally, these bacteria have given rise to a number of new hybrids and variants that are also likely to cause trouble in the future. Indeed, higher levels of evolvability are likely not only to increase the threat from current pathogens, but also "stimulate the emergence of new disease agents" from organisms that used to be our friendly neighbors.
As mentioned earlier, however, evolvability should be found at relatively lower levels in systems where it leads to more harm than good--for instance, places where there is limited exposure to novel antibiotic products. It is unlikely that we will be able to easily remove current contamination, but we can limit the amount introduced in the future by minimizing unnecessary use of antimicrobials and by disposing of them in a more eco-friendly way. This won't stop bacteria from developing defenses against our drugs and disinfectants, but it might help reduce the speed with which they do so.
---
Click here to visit the Anthrophysis Facebook page!
Gillings, M.R., and Stokes, H.W. 2012. Are humans increasing bacterial evolvability? Trends in Ecology and Evolution, 27(6): online advance publication.
Thanks to the following websites for providing the images used in this post:
http://en.wikipedia.org/wiki/File:CDC-10046-MRSA.jpg
http://en.wikipedia.org/wiki/Acinetobacter_baumannii

No comments:
Post a Comment